
In March 2020, the World Health Organization declared COVID-19 a pandemic after early Covid-19 infection cases immediately spread to 118,000 people in 114 countries in just a short period of time. As of now, there have been a total of more than 4.55 million deaths out of the more than 219 million recorded cases.
COVID-19, also known as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), emerged in late 2019 in the city of Wuhan, which is located at Hubei Province, China. The International Committee of Taxonomy of Viruses created its name after sequencing the virus’s genome and discovering that it is genetically related to the 2003 SARS outbreak.
Though it’s still a mystery where COVID-19 came from, it has dramatically changed the world in which we live in multiple ways. Our working arrangements have shifted. Many of us turned into work-from-home employees. There are now fewer commuters and virtual conference calls have become the new normal. International travel has also become restricted as borders closed one after the other to stop the virus from spreading.
More than a year after being designated as a pandemic, countries are now frantically working on getting their citizens vaccinated. The world is currently on a mission to create the safest and most effective COVID-19 vaccine. As of now, there are 22 authorized and approved vaccines around the globe, including Pfizer, Moderna, AstraZeneca, Sputnik V, Comirnarty, and CoronaVac. But there are another 91 candidates in development.
Still, various studies and research have found that, aside from vaccines, it is essential to detect and treat early COVID-19 infection to save more lives.
What COVID-19 does
For as yet unknown reasons, COVID-19 has different effects on people. Some remain asymptomatic. Others suffer only mild symptoms. On the other hand, many end up in hospitals and, tragically, many do not survive. Scientists are still trying to find out why people don’t react the same way towards COVID-19. But despite not knowing all the answers, experts have a growing understanding of how the virus attacks.
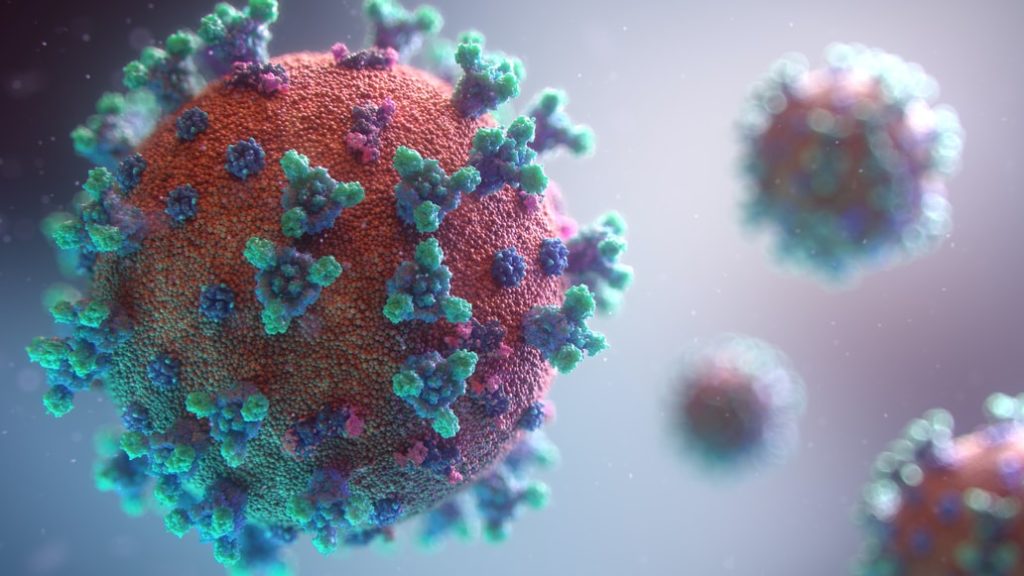
COVID-19 takes hold just like any of the other coronaviruses. It enters our body when a person infected with the virus coughs or sneezes. These external responses result in microscopic respiratory droplets containing spiked proteins that attach themselves to the cells lining our eyes, mouth, nose, and throat. They then take over these cells and turn them into viruses, contaminating the adjacent cells.
This process stops where it started in some people and will only give them a sore throat or runny nose. But if the person’s immune system fails to protect the body, as happens in many cases, the virus continues to spread further and affects the olfactory nerve and taste buds, taking away the sense of smell and flavor detection. It can also go straight to our respiratory tract where sufferers experience a painful, dry cough.
The worst-case scenario is when the virus reaches our lungs.
Once the virus is in the lungs, it causes inflammation that can result in severe, life-threatening respiratory issues such as pneumonia and acute respiratory distress syndrome (ARDS). Eventually, the lungs will fill with fluids, making it difficult to breathe. When this happens, respiratory failure is imminent. Patients will need ventilators and intubation in order to maintain oxygen supply.
Detecting COVID-19 early
It is now abundantly clear that early detection of COVID-19 is essential to prevent further infections, severe illness, and death. It can also help alleviate the heavy demands on healthcare systems. This is what National Institute of Allergy and Infectious Diseases (NIAID) Director Anthony S. Fauci, M.D., and his colleagues asserted in their JAMA Viewpoint article last November 2020.
A lot of people who start with mild symptoms find themselves ending up in hospitals. If they survive, it’s likely that they may suffer life-long health complications such as heart and lung conditions. To mitigate these effects, COVID-19 has to be treated at its earliest stages whenever possible. Early detection will also help reduce the likelihood of spreading the virus to more people, which is known to increase the risk of new variants emerging.
A study by the University of Illinois at Urbana-Champaign published in June 2021 on ScienceDaily reiterates that testing is still the best way to detect the virus as early as possible. The findings state that there is 98% sensitivity to identifying COVID-19 if polymerase chain reaction (PCR) and antigen tests work with rapid result reporting. They also highlight that PCR is the most accurate and effective test so far when it comes to spotting COVID-19 cases.
PCR tests have the capacity to find the virus even before patients acquire an infectious viral load. Thus, these patients can be isolated as soon as possible. They will not only avoid infecting others but they will also be given treatment right away.
The study insists that it’s still the most essential tool in detecting COVID-19 at its earliest. This is especially the case with countries where the administration of vaccines is not yet widely implemented. However, if PCR tests and rapid result reporting aren’t available, using cheaper rapid testing should be conducted about three times a week to increase the sensitivity rate.
The need to treat early COVID-19 infection
More than 18 months into the pandemic, there are still no specific treatments against COVID-19. However, there are drugs that have saved critically-affected patients, including baricitinib, dexamethasone, remdesivir, and tocilizumab. Unfortunately, these drugs can only be given to help patients who have symptoms that are severe enough to cause hospitalization. They cannot be used in people with mild or early COVID-19 stages.
In other words, there is still no approved COVID-19 cure for patients who do not meet hospitalization criteria. Every research effort meant for it has met with setbacks. There are cases of false leads and a lack of participants in outpatient studies. Moreover, when the pandemic started, most of the scientific efforts were focused on hospital treatments for severe cases rather than mild ones, and that remains the case to this day.
Fortunately, several studies are still ongoing and some of them look promising. For instance, there are orally administered drugs like the antiviral drug molnupiravir and antidepressant pill fluvoxamine that are being studied. The pandemic is still far from over. Whether or not they will yield great results, experts still consider them as progress and a few steps closer to success.
In the meantime, COVID-19 vaccination campaigns in addition to rigorous early testing remain the best defenses against the pandemic as we wait for drugs that can cure early COVID-19 infection.






